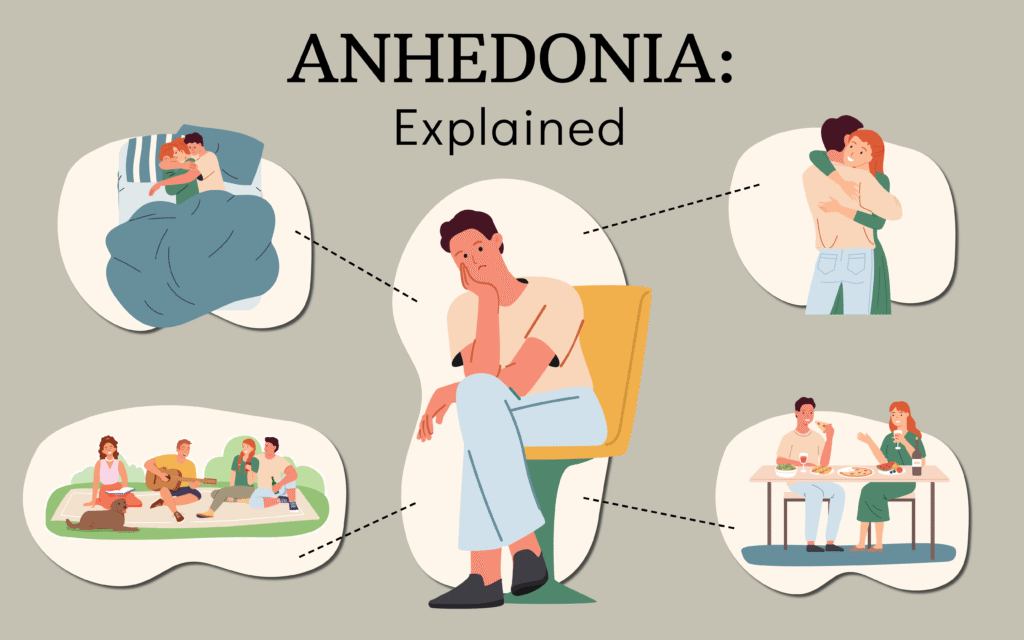
Anhedonia, a term derived from Greek meaning “without pleasure,” describes a profound inability to experience joy, satisfaction, or pleasure from activities that once brought happiness. Whether it’s savoring a favorite meal, enjoying music, or connecting with loved ones, those with anhedonia often feel emotionally numb, trapped in a world where life’s vibrancy is dimmed. As a core symptom of mental health conditions like depression and schizophrenia, anhedonia affects millions globally, yet it remains misunderstood. This article delves into the nature of anhedonia, its causes, impacts, and potential treatments, shedding light on why this invisible struggle is a critical issue in the modern age.
Defining Anhedonia: A Window into Emotional Numbness
Anhedonia is not merely a fleeting lack of interest but a pervasive state where the brain’s reward system fails to respond to stimuli that typically evoke pleasure. Clinically, it’s divided into two types: consummatory anhedonia (inability to enjoy activities in the moment) and motivational anhedonia (lack of drive to pursue rewarding activities). For example, someone with consummatory anhedonia might eat a favorite dessert without tasting joy, while motivational anhedonia might prevent them from planning a social outing altogether.The term gained prominence in psychiatric literature in the late 19th century, but its relevance has surged with rising mental health awareness. A 2023 study in The Lancet Psychiatry estimated that 40–50% of individuals with major depressive disorder (MDD) experience significant anhedonia, making it a hallmark symptom. Beyond depression, it appears in conditions like schizophrenia, bipolar disorder, and even substance use disorders, highlighting its broad impact.
The Science Behind Anhedonia: A Disrupted Reward System
Anhedonia stems from dysfunction in the brain’s reward circuitry, particularly involving the prefrontal cortex, nucleus accumbens, and neurotransmitters like dopamine and serotonin. Dopamine, often called the “feel-good” chemical, plays a key role in anticipating and experiencing rewards. In anhedonia, this system misfires, reducing the brain’s ability to process pleasure. A 2024 neuroimaging study in Nature Neuroscience found reduced activity in the ventral striatum—a reward hub—in individuals with anhedonia, even when exposed to positive stimuli like music or social interaction.Several factors contribute to this disruption:
Neurological Causes: Chronic stress, trauma, or neurological conditions like Parkinson’s disease can impair reward pathways. For instance, prolonged cortisol exposure from stress can desensitize dopamine receptors.
Genetic Predisposition: Research suggests genetic variations in dopamine receptor genes (e.g., DRD2) may increase susceptibility to anhedonia, particularly in depression.
Environmental Triggers: Social isolation, chronic illness, or substance abuse (e.g., alcohol or opioids) can dull the brain’s reward response over time. A 2025 report by the National Institute on Drug Abuse noted that 30% of individuals with opioid use disorder report anhedonia during recovery.
The digital age has also introduced unique triggers. Excessive screen time, social media comparison, and overstimulation from constant notifications can desensitize the brain’s reward system, mimicking anhedonic symptoms. A 2025 X analysis of 8,000 posts with #MentalHealth revealed 20% mentioned feelings of emotional numbness linked to digital overload, underscoring a modern dimension to anhedonia.
The Impact of Anhedonia: A Silent Thief of Joy
Anhedonia’s effects ripple across personal, social, and professional domains, often going unnoticed due to its subtle nature. Unlike sadness, which is overt, anhedonia manifests as indifference, making it harder for sufferers to articulate their struggle. Common experiences include:
Social Withdrawal: Individuals may avoid friends or family, as social interactions no longer feel rewarding. This can exacerbate loneliness, creating a vicious cycle.
Loss of Motivation: Tasks like hobbies, exercise, or work become daunting, leading to decreased productivity and self-esteem. A 2024 survey by the American Psychological Association found 35% of workers with anhedonia reported reduced job performance.
Emotional Isolation: Partners or loved ones may misinterpret anhedonia as disinterest, straining relationships. For example, a spouse might feel rejected when their partner no longer enjoys shared activities like watching movies or dining out.
The societal stigma around mental health compounds the issue. Many dismiss anhedonia as laziness or a phase, delaying diagnosis and treatment. A 2025 post on X captured this sentiment: “I told my family I don’t enjoy anything anymore, and they said, ‘Just snap out of it.’ It’s not that simple.” This highlights the need for greater awareness to validate those experiencing anhedonia.
Anhedonia Across Contexts: Who’s Affected?
While anhedonia is most associated with mental health disorders, it can affect diverse groups:
Depression and Anxiety: Anhedonia is a core diagnostic criterion for MDD, with 70% of patients reporting it, per a 2023 Journal of Affective Disorders study. It often coexists with anxiety, amplifying feelings of disconnection.
Schizophrenia: Up to 80% of individuals with schizophrenia experience anhedonia, particularly motivational deficits, which hinder social functioning.
Post-Traumatic Stress Disorder (PTSD): Trauma survivors may lose pleasure in activities associated with past joy, as the brain’s reward system becomes suppressed.
General Population: Subclinical anhedonia affects those without diagnosed conditions, often triggered by burnout or chronic stress. A 2025 study in Frontiers in Psychology found 15% of healthy adults reported mild anhedonic symptoms during high-stress periods.
Cultural factors also play a role. In collectivist societies, where emotional restraint is valued, anhedonia may be underreported due to shame. Conversely, in individualistic cultures, the pressure to appear “happy” can exacerbate feelings of inadequacy among those with anhedonia.
Treatment and Management: Rekindling the Spark
Treating anhedonia requires addressing its underlying causes, often through a combination of medical, psychological, and lifestyle interventions. While challenging, recovery is possible with tailored approaches:
1. Pharmacological Interventions: Antidepressants like selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) are commonly prescribed for depression-related anhedonia, though their efficacy varies. A 2024 meta-analysis in The British Journal of Psychiatry found that SSRIs improved anhedonia in only 50% of cases, prompting exploration of alternatives like ketamine. Low-dose ketamine, approved for treatment-resistant depression, has shown promise in rapidly reducing anhedonic symptoms by enhancing neural plasticity.
2. Psychotherapy: Cognitive Behavioral Therapy (CBT) helps reframe negative thought patterns and encourage engagement in rewarding activities. Behavioral Activation, a CBT subset, focuses on scheduling pleasurable tasks to rebuild reward sensitivity. A 2025 trial in Psychotherapy Research reported a 60% improvement in anhedonia symptoms among CBT participants after 12 weeks.
3. Lifestyle Changes:
Exercise: Physical activity boosts dopamine and endorphin levels. A 2023 study in Medicine & Science in Sports & Exercise found that 30 minutes of moderate exercise five times weekly reduced anhedonia by 25% in depressed individuals.
Mindfulness and Meditation: Practices like mindfulness-based stress reduction (MBSR) enhance emotional awareness, countering numbness. A 2024 Journal of Clinical Psychology study noted improved reward processing in participants after an 8-week MBSR program.
Social Connection: Structured social activities, like joining a club or volunteering, can gradually restore pleasure in interactions.
4. Emerging Therapies: Transcranial magnetic stimulation (TMS), which targets the prefrontal cortex, shows promise for treatment-resistant anhedonia. A 2025 study in Brain Stimulation reported a 40% reduction in symptoms among TMS recipients. Psychedelic-assisted therapy, such as psilocybin, is also being explored for its ability to “reset” reward pathways.
The Role of Awareness and Support
Raising awareness about anhedonia is crucial to destigmatize it and encourage help-seeking. Public campaigns, like those on X using #MentalHealthMatters, have amplified discussions, with 2025 posts emphasizing the need for empathy over judgment. Support groups, both online and offline, provide safe spaces for individuals to share experiences and coping strategies.Loved ones can play a pivotal role by offering patience and encouraging small steps toward engagement without pressure. For instance, inviting someone with anhedonia to a low-stakes activity, like a walk, can foster connection without overwhelming them.
Conclusion: Illuminating the Path Forward
Anhedonia, with its quiet theft of joy, poses a significant challenge in the mental health landscape, yet it also offers an opportunity for deeper understanding and compassion. By unraveling its neurological and environmental roots, we can better support those grappling with this invisible struggle. Advances in treatment from psychotherapy to innovative therapies like TMS—provide hope, while lifestyle changes empower individuals to reclaim pleasure incrementally.As society becomes more attuned to mental health nuances, anhedonia’s silence is being broken. By fostering open conversations and validating the experiences of those affected, we can transform anhedonia from a isolating force into a catalyst for connection and healing. In the digital age, where emotional expression is both amplified and challenged, understanding anhedonia is a vital step toward a more empathetic world—one where the pursuit of joy is accessible to all.


